Understanding Gibbs Injuries

A Gibbs injury, also known as a “reverse Hill-Sachs lesion,” is a specific type of fracture-dislocation that occurs in the shoulder joint. It’s named after Dr. Gibbs, a surgeon who first described this injury.
Mechanism of a Gibbs Injury
Gibbs injuries occur when the humeral head, the ball-shaped upper end of the arm bone, is forced backward against the glenoid, the socket of the shoulder joint. This happens when the arm is forcefully abducted (raised away from the body) and externally rotated. The impact can cause a fracture of the posterior (back) part of the humeral head, creating a characteristic “bump” or indentation.
Types of Gibbs Injuries
Gibbs injuries can be classified into different types based on the severity and location of the fracture.
* Type 1: A small, isolated fracture of the posterior humeral head.
* Type 2: A larger fracture that extends into the articular surface of the humeral head.
* Type 3: A complete fracture of the posterior humeral head, involving significant bone displacement.
Presentation of a Gibbs Injury
A Gibbs injury typically presents with a combination of signs and symptoms.
* Pain: Intense pain in the shoulder, particularly when moving the arm.
* Swelling: Visible swelling around the shoulder joint.
* Instability: A feeling of instability or “giving way” in the shoulder.
* Limited Range of Motion: Difficulty in moving the arm in various directions.
* Deformity: A noticeable bump or indentation in the back of the shoulder.
* Crepitus: A grating or crunching sound when moving the arm.
* Locking: The arm may lock in a particular position, making it difficult to move.
* Weakness: Decreased strength in the shoulder and arm muscles.
Gibbs injuries can be challenging to diagnose, as the symptoms can be similar to other shoulder injuries. A thorough physical examination, imaging studies such as X-rays and MRI scans, and a detailed medical history are essential for accurate diagnosis.
Diagnosis and Treatment: Gibbs Injury
Diagnosing and treating a Gibbs fracture requires a multi-pronged approach, combining medical expertise with advanced imaging techniques. Understanding the nuances of this injury is crucial for effective management and optimal patient outcomes.
Imaging Techniques, Gibbs injury
Imaging plays a critical role in identifying a Gibbs fracture and guiding treatment decisions. These techniques provide visual evidence of the injury’s extent and location.
- X-ray: This is often the first imaging test performed. It provides a clear view of the bones and helps identify any fractures or dislocations. However, X-rays may not always be sufficient to fully assess the extent of a Gibbs fracture, particularly if the fracture is subtle or involves soft tissues.
- Computed Tomography (CT) Scan: A CT scan provides detailed, three-dimensional images of the bones and surrounding tissues. It can be especially helpful in visualizing complex fractures, including those involving the articular surface (the smooth surface of a joint) and soft tissues.
- Magnetic Resonance Imaging (MRI): An MRI scan provides detailed images of soft tissues, including ligaments, tendons, and cartilage. It is particularly useful for evaluating injuries to the ligaments and tendons associated with a Gibbs fracture, which may not be visible on X-ray or CT scans.
Clinical Examination
In addition to imaging, a thorough clinical examination is essential for diagnosing a Gibbs fracture. This involves a detailed assessment of the patient’s symptoms, including:
- Pain: The patient will typically experience pain in the affected area, which may worsen with movement.
- Swelling: Swelling around the injury site is common, as the body’s natural response to injury is inflammation.
- Tenderness: The area around the fracture will be tender to the touch.
- Limited Range of Motion: The patient may experience difficulty moving the affected joint due to pain and instability.
- Deformity: A visible deformity may be present, depending on the severity of the fracture.
Treatment Options
Treatment for a Gibbs fracture depends on the severity of the injury, the patient’s age, and their overall health.
- Conservative Management: For less severe Gibbs fractures, conservative treatment may be sufficient. This typically involves:
- Rest: Limiting movement and weight-bearing on the affected joint to allow the fracture to heal.
- Ice: Applying ice packs to the injured area to reduce swelling and pain.
- Compression: Using a compression bandage to reduce swelling and provide support.
- Elevation: Keeping the injured limb elevated to help reduce swelling.
- Pain Medication: Over-the-counter pain relievers, such as ibuprofen or acetaminophen, can help manage pain.
- Physical Therapy: Once the initial pain and swelling have subsided, physical therapy can help restore range of motion and strength in the affected joint.
- Surgical Intervention: For more severe Gibbs fractures, surgery may be necessary to restore stability and proper alignment of the joint. Surgical options may include:
- Open Reduction and Internal Fixation (ORIF): This procedure involves surgically exposing the fracture, realigning the bone fragments, and fixing them in place with plates, screws, or other implants.
- Arthrodesis: In some cases, particularly for severely unstable fractures, the joint may need to be fused (arthrodesis). This involves surgically joining the bones together, eliminating the joint and reducing the risk of further injury.
Effectiveness of Treatment Approaches
The effectiveness of different treatment approaches for Gibbs fractures depends on several factors, including the severity of the injury, the patient’s age and health, and the skill of the treating physician.
- Conservative Management: Conservative treatment is generally effective for less severe Gibbs fractures. However, it may not be suitable for all patients, especially those with significant instability or displacement of the fracture fragments.
- Surgical Intervention: Surgical intervention is often necessary for more severe Gibbs fractures, as it can provide greater stability and improve the chances of a successful outcome. However, surgery carries risks, such as infection, bleeding, and nerve damage.
Rehabilitation and Recovery

Recovering from a Gibbs injury is a journey that requires patience, dedication, and a strong support system. The rehabilitation process aims to restore function, reduce pain, and prevent long-term complications. It’s a collaborative effort involving medical professionals, therapists, and the patient themselves.
Physical Therapy
Physical therapy plays a crucial role in regaining strength, flexibility, and mobility after a Gibbs injury. Therapists design personalized exercise programs tailored to the individual’s needs and limitations.
- Range of Motion Exercises: These exercises help to restore flexibility and prevent stiffness in the affected joints.
- Strengthening Exercises: These exercises focus on building muscle strength in the injured area and surrounding muscles to support the joint.
- Balance and Coordination Exercises: These exercises help improve stability and coordination, which are essential for safe movement and activities.
- Proprioceptive Exercises: These exercises help retrain the brain and body to sense and control movement.
Occupational Therapy
Occupational therapy focuses on improving daily living skills and activities. Therapists work with patients to address specific challenges they face due to their injury.
- Adaptive Equipment: Therapists may recommend and train patients on using adaptive equipment, such as assistive devices, to make daily tasks easier.
- Ergonomic Training: Therapists provide guidance on proper body mechanics and ergonomics to prevent further injury and promote safe movement during daily activities.
- Cognitive Rehabilitation: For patients experiencing cognitive difficulties due to their injury, therapists may incorporate cognitive exercises to improve memory, attention, and problem-solving skills.
Importance of Early Intervention
Early intervention is crucial for maximizing recovery potential and minimizing long-term complications. Delayed treatment can lead to:
- Increased Pain and Stiffness: Delayed treatment can allow pain and stiffness to worsen, making rehabilitation more challenging.
- Limited Range of Motion: Prolonged inactivity can lead to decreased range of motion in the affected joints, hindering functional recovery.
- Increased Risk of Secondary Injuries: Delayed treatment can increase the risk of developing secondary injuries, such as muscle imbalances or joint instability.
Success Stories
Many individuals have successfully recovered from Gibbs injuries with dedication and commitment to their rehabilitation programs. One example is a young athlete who suffered a severe Gibbs injury during a football game. He underwent surgery and followed a rigorous physical therapy program, demonstrating remarkable progress. He was able to return to competitive sports within a year, highlighting the importance of patient compliance and motivation in achieving successful outcomes.
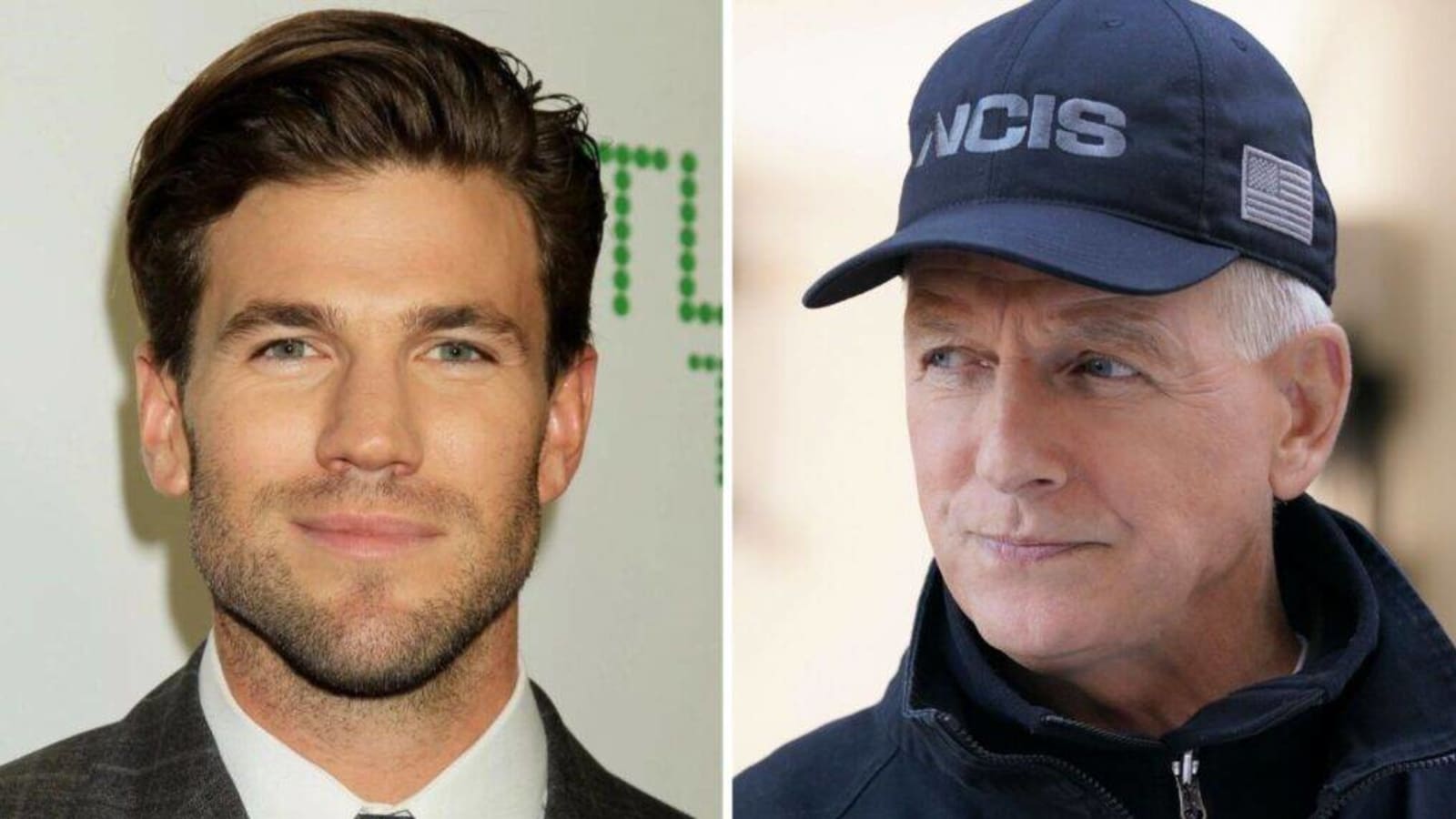
Gibbs injury – While Gibbs’s injury may have been a bit of a scare, it’s nothing compared to the agony of a torn meniscus. A torn meniscus, as you can read about here , can leave you limping around like a wounded gazelle.
Thankfully, Gibbs’s injury appears to be minor, and he should be back to his usual, gruff self in no time.
The news of Gibbs’ injury has sent shockwaves through the team, leaving fans wondering who will step up in his absence. Luckily, the Wolverines have a rising star in JJ McCarthy, whose impressive stats can be found here.
While McCarthy may not be a direct replacement for Gibbs, his potential could certainly help fill the void and keep the team in contention.
